Let’s start with the first steps…getting connected with a JFCS therapist.
When you first call for a therapy appointment at JFCS, you will speak with our intake coordinator who will ask a few questions to gather some background information to pass along to the therapist with whom your case is assigned.
You will be asked for a general description of why you are coming to therapy – what is called the presenting problem. The reason the intake coordinator asks is to be sure that we are able to provide services for the problem you are dealing with. For example, if someone is experiencing a drug addiction, we would refer them to another provider as we do not provide substance abuse counseling. The intake coordinator is bound by the same HIPPA laws regarding confidentiality and privacy of healthcare information as the therapist.
 When one of our therapists is assigned to you, they will phone you and schedule an initial assessment session which will last for about one hour. This time is a ‘getting to know you’ session, where the therapist will complete what is called a Biopsychosocial Assessment, asking questions to better understand your background, current problems, symptoms, as well as strengths. Oftentimes, more than one session is needed to gather information to conduct a thorough assessment. We don’t want anyone to feel rushed while sharing their personal story of life experiences
When one of our therapists is assigned to you, they will phone you and schedule an initial assessment session which will last for about one hour. This time is a ‘getting to know you’ session, where the therapist will complete what is called a Biopsychosocial Assessment, asking questions to better understand your background, current problems, symptoms, as well as strengths. Oftentimes, more than one session is needed to gather information to conduct a thorough assessment. We don’t want anyone to feel rushed while sharing their personal story of life experiences
At the initial assessment session, paperwork will also be reviewed, such as HIPPA forms, agency policies regarding attendance and other issues. Once the assessment is completed and it is determined that JFCS is the appropriate level of care for your presenting problem, the therapist and client will together develop a Treatment Plan which defines the problem and goals for treatment focus. It is important for both client and therapist to understand what is the ‘endpoint, or when will both know that therapy has been successful.
 What does a typical therapy session look like?
What does a typical therapy session look like?
Therapy can be held individually, as a couple, with a family unit, or in a group with a common treatment focus. Therapy is also available to anyone from childhood to elderly adults. Here at JFCS we can provide therapy services for children starting at age 5 and up to adults of any age.
Sessions are usually held every two weeks and last approximately 45-50 minutes. The length of treatment can vary depending on the complexity of issues which are the focus of treatment. The treatment goals and decisions for how often and how long to meet are collaboratively discussed by the client and therapist.
Currently, for the health and safety of all during the COVID-19 pandemic, all therapy sessions at JFCS are being conducted through video teletherapy on Zoom or by phone. Many other agencies and therapists throughout NJ are also providing services via video teletherapy.
 There are both advantages and drawbacks to this mode of providing therapy. Some of the benefits of engaging in therapy remotely are: there’s no need to travel to an office – you receive services in the comfort of familiar surroundings; it’s an easy process – your therapist emails you a link which you click on at the time of your session to connect for a session. Our team at JFCS has found that clients, overall, have enjoyed the many advantages of video teletherapy.
There are both advantages and drawbacks to this mode of providing therapy. Some of the benefits of engaging in therapy remotely are: there’s no need to travel to an office – you receive services in the comfort of familiar surroundings; it’s an easy process – your therapist emails you a link which you click on at the time of your session to connect for a session. Our team at JFCS has found that clients, overall, have enjoyed the many advantages of video teletherapy.
What would be helpful to know about therapy?
Roles: The relationship between the therapist and client is a professional relationship. This means that the relationship’s purpose is to benefit the client and that there are established boundaries or limits that are deemed appropriate according to the ethical standards set by the therapist’s profession, ex. social work code of ethics. This therapeutic relationship is different from your other relationships. The therapist is bound to keep confidential the information you share with them, with a few exceptions, ex. harming self or others. You can feel confident that what you talk about will stay with your therapist, this may not always be true of your conversations with friends and family.
Therapists reveal very little about themselves to clients, and if they do share something of a personal nature, it needs to be in the service or benefit of the client. The focus of the session is on you, the client; the therapist is there to assist with compassion and without judgment.
While it may seem like a nice idea to be able to continue a relationship outside of the therapy sessions, this is not possible. The therapeutic relationship is not a two-way relationship where both parties get to know each other. The role of the therapist is to help their client, never the other way around. Most therapists genuinely care about their clients and want to see them improve. Establishing healthy boundaries helps with this process.
Guidelines: At the initial session, most therapists will provide information to the client regarding the agency’s policies, such as the cancellation/no show policy, policy related to fees and insurance, how to best contact your therapist between sessions, etc. Discussing this information early on can help to clarify expectations and responsibilities for both client and therapist and help prevent any future misunderstandings. If you have any questions at any time, do not hesitate to bring them up to your therapist.
Expectations: Along with a strong therapeutic relationship, there are several factors that can promote positive therapy outcomes.
- Regular attendance to the sessions
- Being willing to have the “difficult” conversations
- Sharing honestly in session
- Fully participating in therapy
- Being open to feedback
- Completing any tasks or written exercises outside of session
Feeling unsure about therapy?
If you are hesitant about meeting with a therapist, let me share this: Do you think it would be realistic – or a good idea, for a person to go through their entire life, and never see a medical doctor for physical problems? Probably not.
Throughout our life we are bombarded with many outside toxins, viruses, germs, and we also have body parts and systems that wear out or get injured. To alleviate these various illnesses and problems we may need professional help, medical help, to deal effectively with the problem.
It is the same with our mental health. Is it realistic to think that we can go throughout our entire life without needing some professional help for our mental health related problems? Our mental health is just as important as our physical health.
When you are in need of therapy remember that JFCS is here for you. Call 609-987-8100 to schedule an appointment with one of our licensed therapists.
Teri Cheresnick, LCSW, LCADC
 The 2020 election season would have been a stressful one even during normal times but, compounded with a pandemic it is creating, for some, incredible stress and frustration. If you find yourself experiencing what has been described as Election Stress Disorder you are not alone; according to a study recently conducted by the
The 2020 election season would have been a stressful one even during normal times but, compounded with a pandemic it is creating, for some, incredible stress and frustration. If you find yourself experiencing what has been described as Election Stress Disorder you are not alone; according to a study recently conducted by the  When one of our therapists is assigned to you, they will phone you and schedule an initial assessment session which will last for about one hour. This time is a ‘getting to know you’ session, where the therapist will complete what is called a Biopsychosocial Assessment, asking questions to better understand your background, current problems, symptoms, as well as strengths. Oftentimes, more than one session is needed to gather information to conduct a thorough assessment. We don’t want anyone to feel rushed while sharing their personal story of life experiences
When one of our therapists is assigned to you, they will phone you and schedule an initial assessment session which will last for about one hour. This time is a ‘getting to know you’ session, where the therapist will complete what is called a Biopsychosocial Assessment, asking questions to better understand your background, current problems, symptoms, as well as strengths. Oftentimes, more than one session is needed to gather information to conduct a thorough assessment. We don’t want anyone to feel rushed while sharing their personal story of life experiences What does a typical therapy session look like?
What does a typical therapy session look like? There are both advantages and drawbacks to this mode of providing therapy. Some of the benefits of engaging in therapy remotely are: there’s no need to travel to an office – you receive services in the comfort of familiar surroundings; it’s an easy process – your therapist emails you a link which you click on at the time of your session to connect for a session. Our team at JFCS has found that clients, overall, have enjoyed the many advantages of video teletherapy.
There are both advantages and drawbacks to this mode of providing therapy. Some of the benefits of engaging in therapy remotely are: there’s no need to travel to an office – you receive services in the comfort of familiar surroundings; it’s an easy process – your therapist emails you a link which you click on at the time of your session to connect for a session. Our team at JFCS has found that clients, overall, have enjoyed the many advantages of video teletherapy. Why is sunlight so important? Exposure to sunlight is believed to increase a hormone in the brain called serotonin which is associated with boosting your mood and helping you to feel more focused and calmer. The darker lighting at night triggers the brain to make another hormone called melatonin which is responsible for helping you sleep.
Why is sunlight so important? Exposure to sunlight is believed to increase a hormone in the brain called serotonin which is associated with boosting your mood and helping you to feel more focused and calmer. The darker lighting at night triggers the brain to make another hormone called melatonin which is responsible for helping you sleep.  There are many reasons why someone may go to therapy, but a few of the reasons are:
There are many reasons why someone may go to therapy, but a few of the reasons are: Who can provide therapy?
Who can provide therapy? Once you’ve thought about what’s important…
Once you’ve thought about what’s important… Perhaps you’ve never met with a therapist before and are unfamiliar with psychotherapy – or maybe you have participated in therapy and still have some questions about it. Let’s dive into what therapy is all about…
Perhaps you’ve never met with a therapist before and are unfamiliar with psychotherapy – or maybe you have participated in therapy and still have some questions about it. Let’s dive into what therapy is all about… During the COVID-19 pandemic, many organizations, communities, and families have turned to Zoom as a way to connect virtually while remaining socially distant. But joining Zoom calls can be complicated and time-consuming, which discourages us from socializing with relatives and friends. These instructions can help you to join Zoom calls using a computer, a smartphone, or a regular cell phone so that you don’t miss out on virtual social gatherings.
During the COVID-19 pandemic, many organizations, communities, and families have turned to Zoom as a way to connect virtually while remaining socially distant. But joining Zoom calls can be complicated and time-consuming, which discourages us from socializing with relatives and friends. These instructions can help you to join Zoom calls using a computer, a smartphone, or a regular cell phone so that you don’t miss out on virtual social gatherings. September is Hunger Action Month, a time to become educated on food insecurity and gain awareness on how you can help reduce its impact on our community. Although it may not be easily noticeable, food insecurity affects many communities, including Mercer County.
September is Hunger Action Month, a time to become educated on food insecurity and gain awareness on how you can help reduce its impact on our community. Although it may not be easily noticeable, food insecurity affects many communities, including Mercer County.
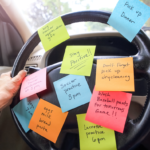 Do you feel overwhelmed by the never-ending list, running like a news ticker-tape across your mind every moment of the day? Does it feel that at the end of the day you’re exhausted physically and mentally, and yet, also that you might have forgot something you were “supposed” to do?
Do you feel overwhelmed by the never-ending list, running like a news ticker-tape across your mind every moment of the day? Does it feel that at the end of the day you’re exhausted physically and mentally, and yet, also that you might have forgot something you were “supposed” to do?
