Addressing the Silent Epidemic: Food Insecurity in Mercer County
Guest Op-Ed Published in The Trentonian November 21, 2023
In the heart of New Jersey lies a shadowed reality that often goes unnoticed amidst our thriving communities—the silent epidemic of food insecurity. Mercer County, a region known for its cultural diversity and economic vitality, faces an escalating crisis that demands immediate attention.
As the Covid pandemic recedes, we are seeing the rapid spread of food insecurity across our region. Amidst our picturesque landscapes and vibrant neighborhoods, thousands of families grapple with the uncertainty of their next meal. Food insecurity, a multifaceted issue, extends its reach into the lives of increasing numbers of the vulnerable—the elderly, children, and working-class families struggling to make ends meet.
The magnitude of this crisis has been exacerbated by recent events, including soaring living costs, the end of pandemic relief programs, a lack of affordable housing, and unforeseen challenges facing many families.
Statistics paint a stark reality. Over 10% of Mercer County residents are food insecure, and they live in every part of our county. That means there is a 100% chance that someone who is hungry is your neighbor. The problem is even more acute in places like our Capital City where 27% of Trenton residents – and 37% of Trenton children – are living below the poverty line.
The face of hunger reflects the full range of diversity in our County. It’s children in our classrooms, unable to concentrate due to an empty stomach. It’s hardworking parents juggling bills and groceries, forced to make agonizing choices between nutrition and other necessities. It’s far too many senior citizens quietly battling hunger while living on a fixed income. These faces are more than just statistics. They are our neighbors, our family members, and our future.
The recent growth in food insecurity in Mercer County is unprecedented. Our organizations have been combatting food insecurity in Mercer County for decades, and we have never seen as many people seeking food assistance as we have in recent months. It’s traditional to focus concern on hunger at this time of year, but this is a continuing challenge that will be with us long after the holidays are over. Food insecurity like the chronic health conditions it can cause, has become chronic.
Our organizations are at the forefront of this crisis, attempting to meet the increasing need with dignity and compassion. Through our experience, we know what works. Our organizations offer nourishment, both through hot meals and food assistance. We provide pathways to self-sufficiency through education, housing, and workforce development. We measure our success not by the number of meals we serve or the amount of food assistance we provide, but by the number of people who no longer need our services.
New Jersey has taken important steps to support those facing hunger, including increasing benefits under the Supplemental Nutrition Assistance Program (SNAP), expanding food assistance programs, and creating the Office of the Food Security Advocate. We are grateful for this leadership by the State to address food insecurity.
The surging demand across Mercer County is outpacing these resources, highlighting the need for a comprehensive, community-driven approach. Our organizations have committed to work collaboratively to empower our communities and advance equity to reduce food insecurity throughout Mercer County. Only by developing a shared strategy and working in alignment can we achieve this ambitious goal. We hope to enlist support from corporate partners, foundations, and the broader community to invest in these innovative efforts.
The time to act is now. Mercer County is at a crossroads, and our response will define the future and the collective values of our community. The fight against food insecurity is not insurmountable but requires our unwavering commitment and concerted efforts.
That is why our organizations have pledged to work together to address this critical issue. By standing together, advocating for change, and extending a hand to those in need, we can create a brighter, more nourished tomorrow for all.
Joyce E. Campbell, CEO of Trenton Area Soup Kitchen
Bernie Flynn, CEO of Mercer Street Friends
David Fox, Executive Director of Arm in Arm
Michelle Napell, Executive Director of Jewish Family & Children’s Services
Sarah Steward, CEO of HomeFront
Barrett Young, CEO of Rescue Mission of Trenton




 their mental and physical health. In addition, practicing breathing techniques can reduce stress. This can be taught by inhaling slowly through the nose, holding the breath for a count of four and then exhaling slowly.
their mental and physical health. In addition, practicing breathing techniques can reduce stress. This can be taught by inhaling slowly through the nose, holding the breath for a count of four and then exhaling slowly. Shopping at the grocery store these days shows us how the
Shopping at the grocery store these days shows us how the 
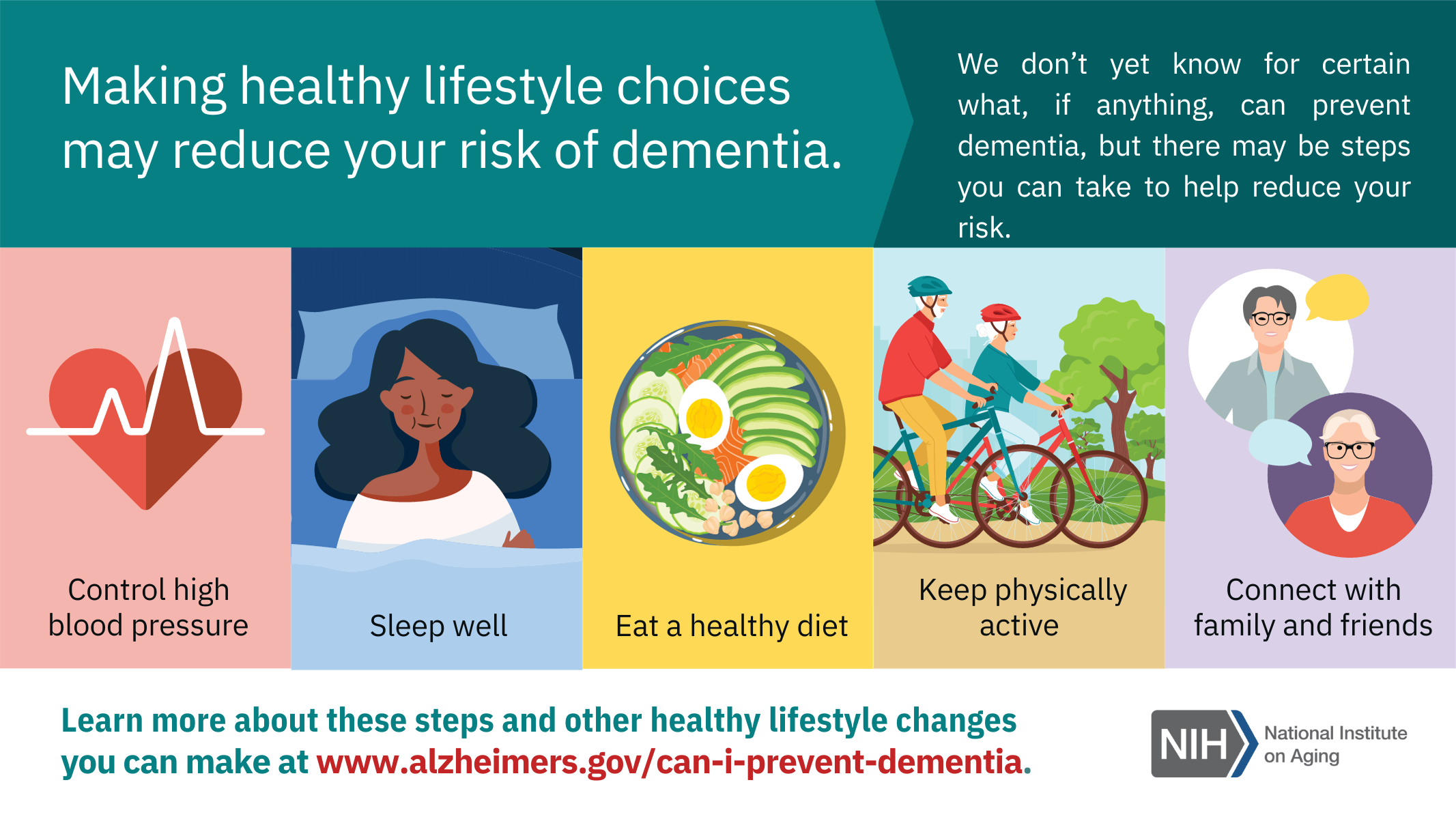
 Participate in JFCS’ 2nd Annual Wheels for Meals bike ride on October 9th! Funds raised support all JFCS food distribution programs including the brick-and-mortar and mobile food pantries and senior nutrition programs. With several route options for beginners to the most experienced cyclists, this ride has something for everyone! Not a rider? Sponsor one or donate to the event. Learn more and register to ride at
Participate in JFCS’ 2nd Annual Wheels for Meals bike ride on October 9th! Funds raised support all JFCS food distribution programs including the brick-and-mortar and mobile food pantries and senior nutrition programs. With several route options for beginners to the most experienced cyclists, this ride has something for everyone! Not a rider? Sponsor one or donate to the event. Learn more and register to ride at 



