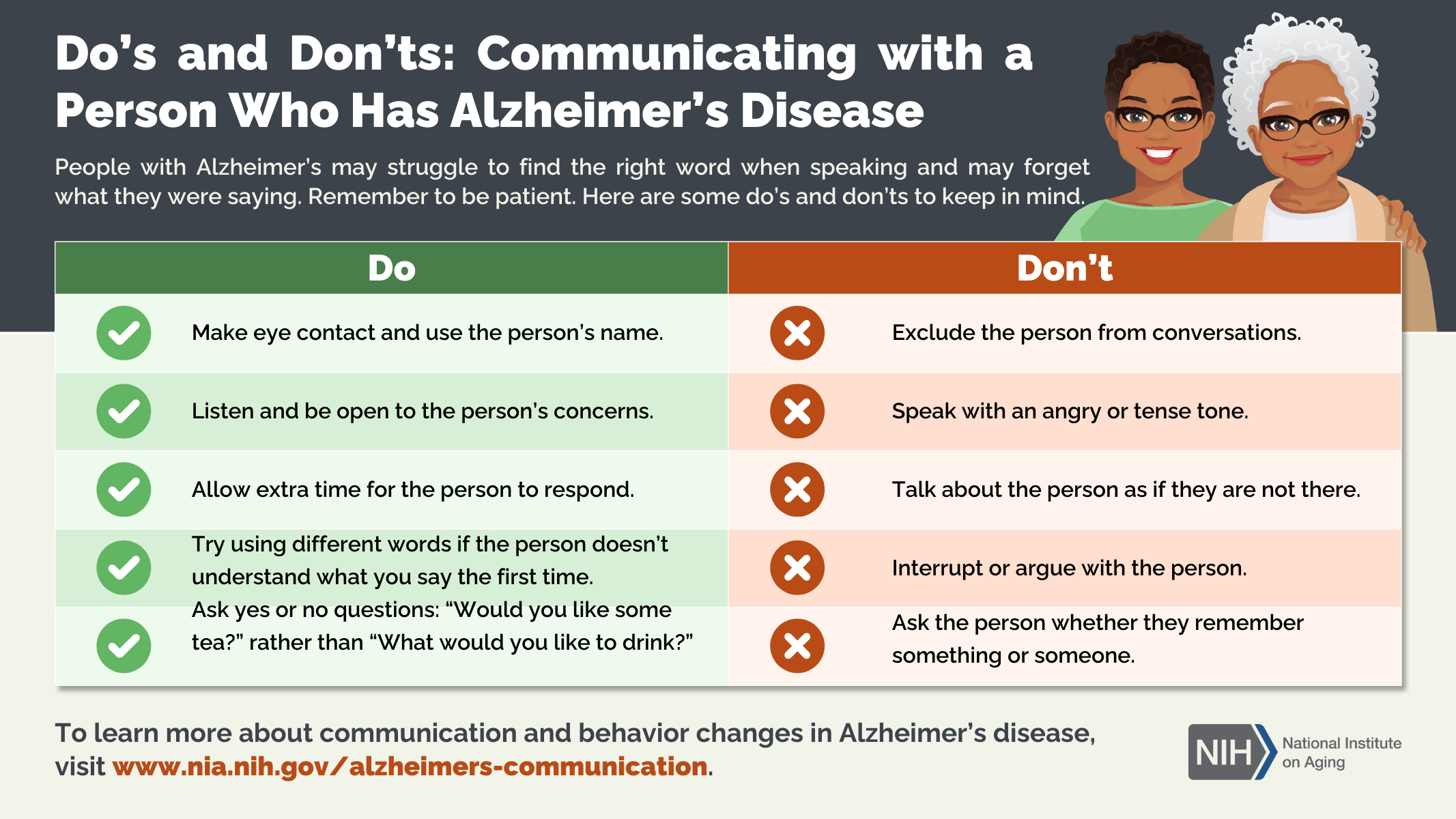
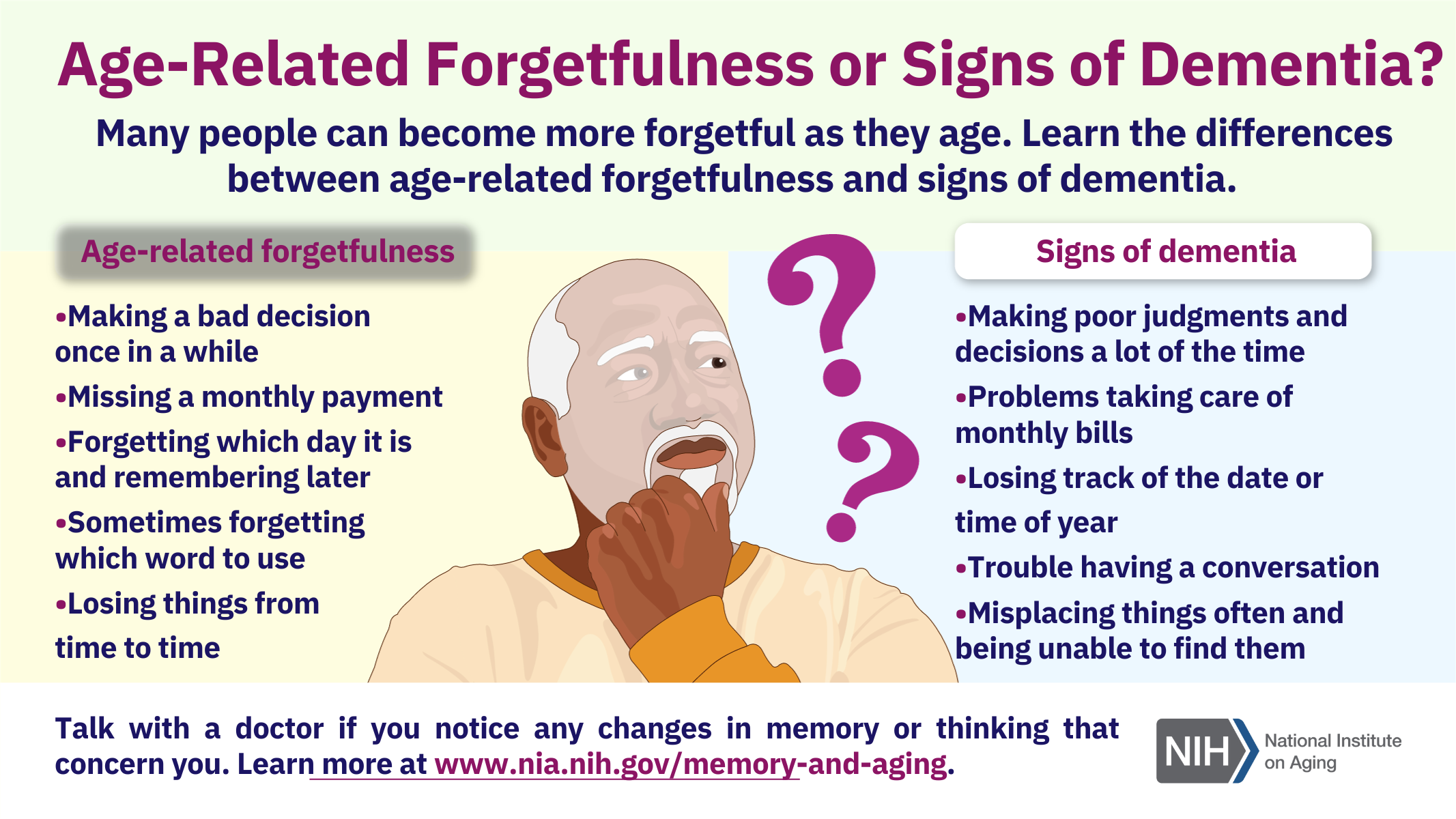
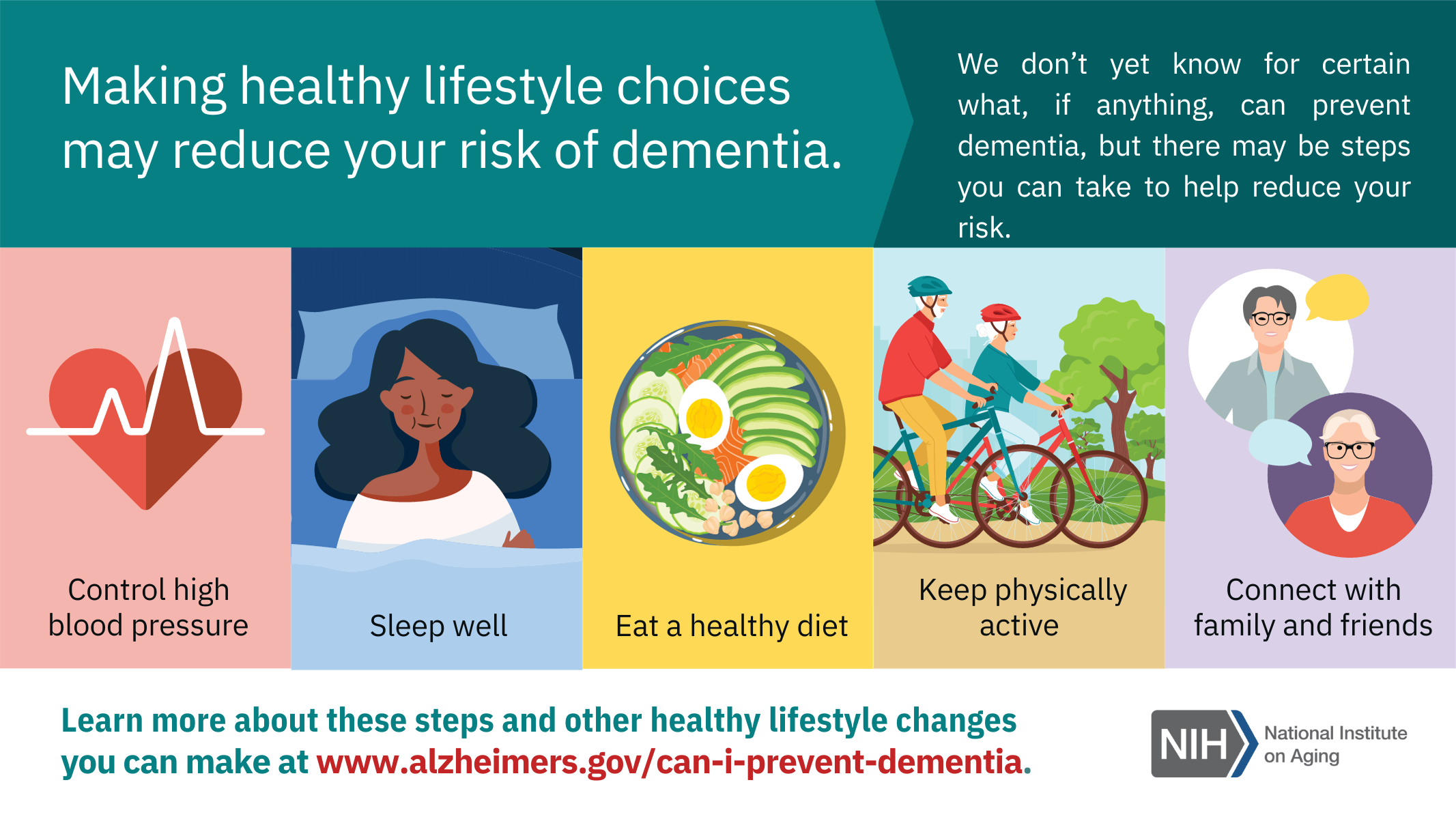
Resources for Alzheimer’s Disease Awareness
November was officially marked as Alzheimer’s Disease Awareness Month. Below are a few infographic resources available through the National Institute on Aging.
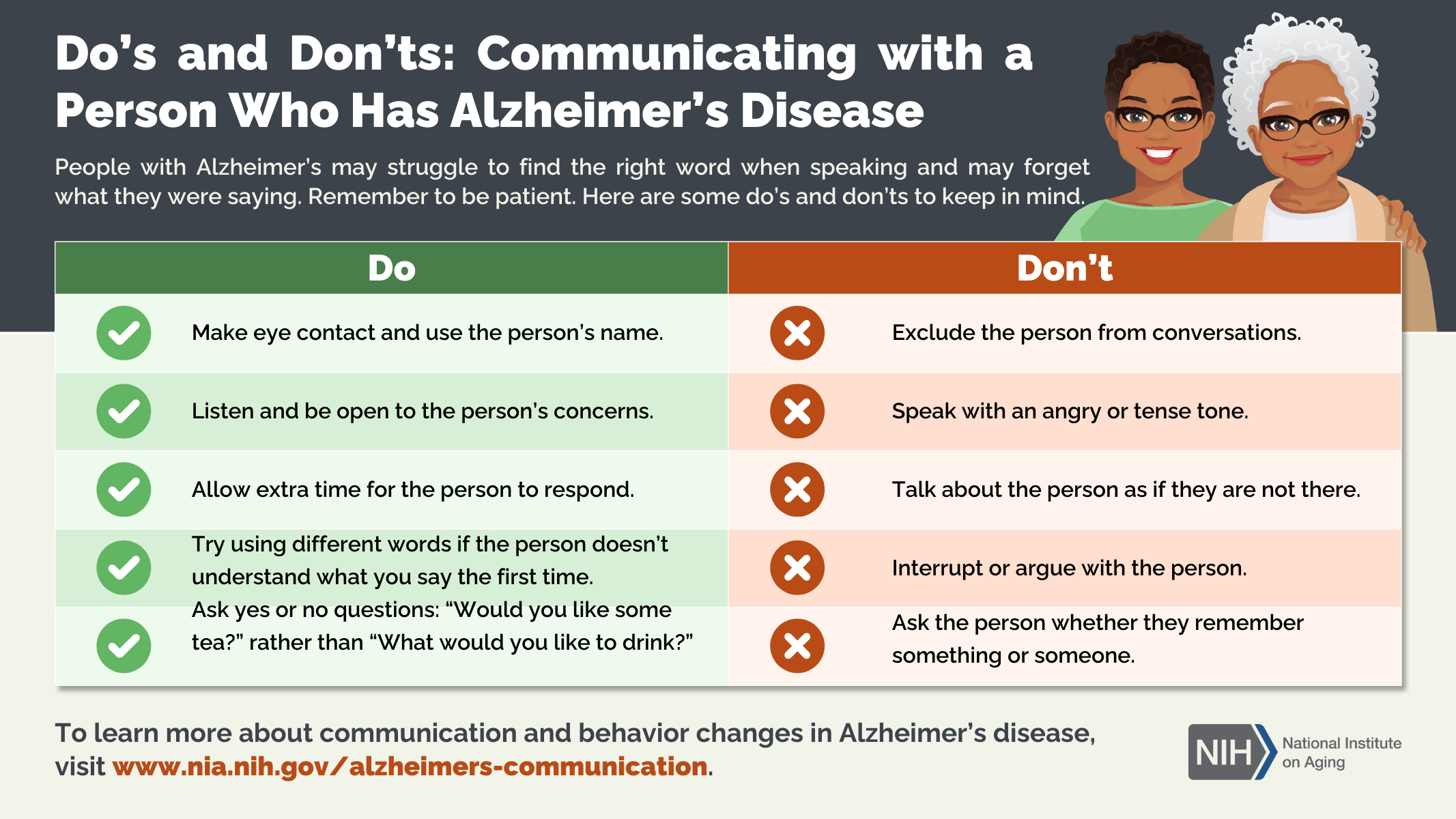
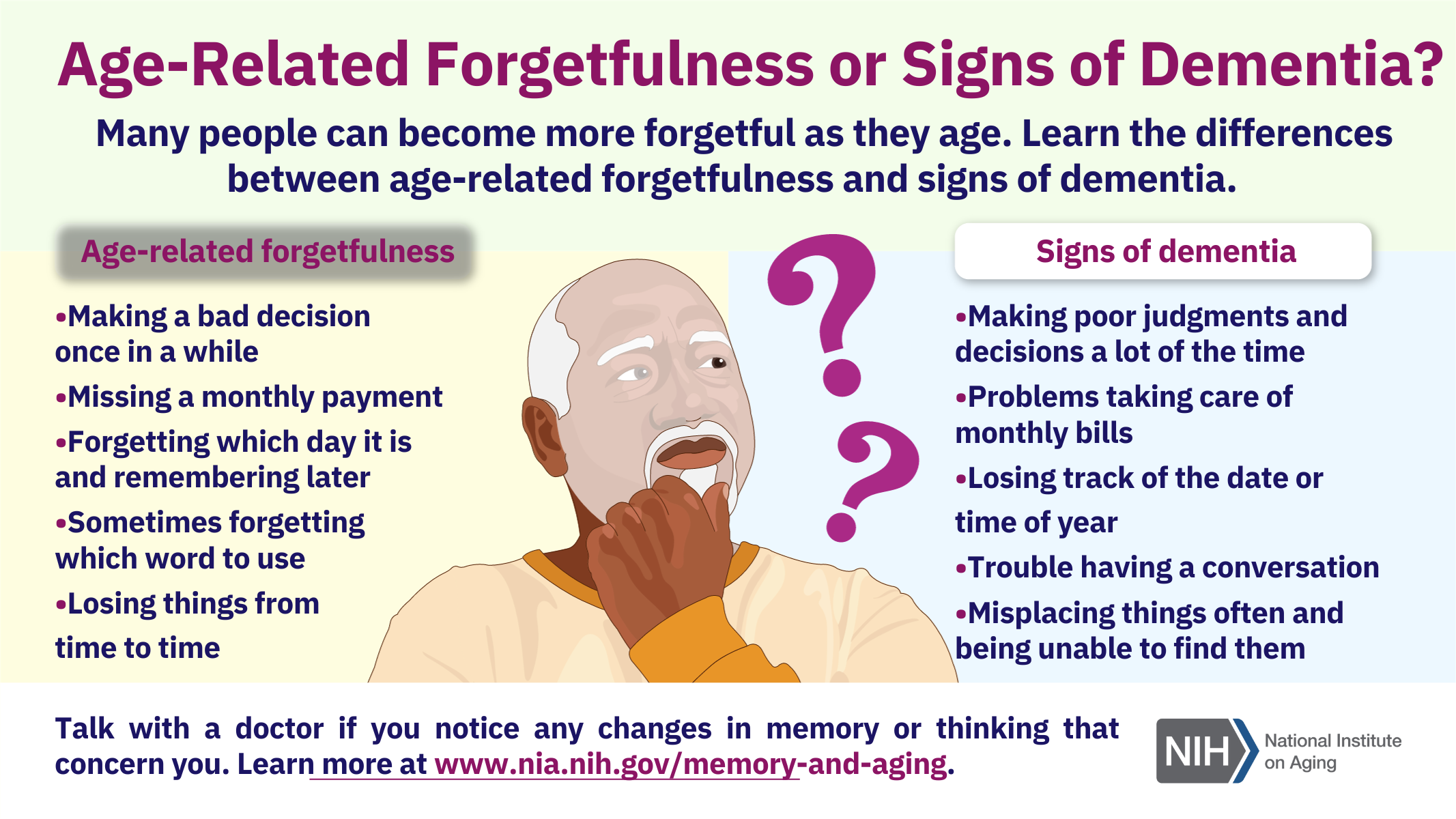

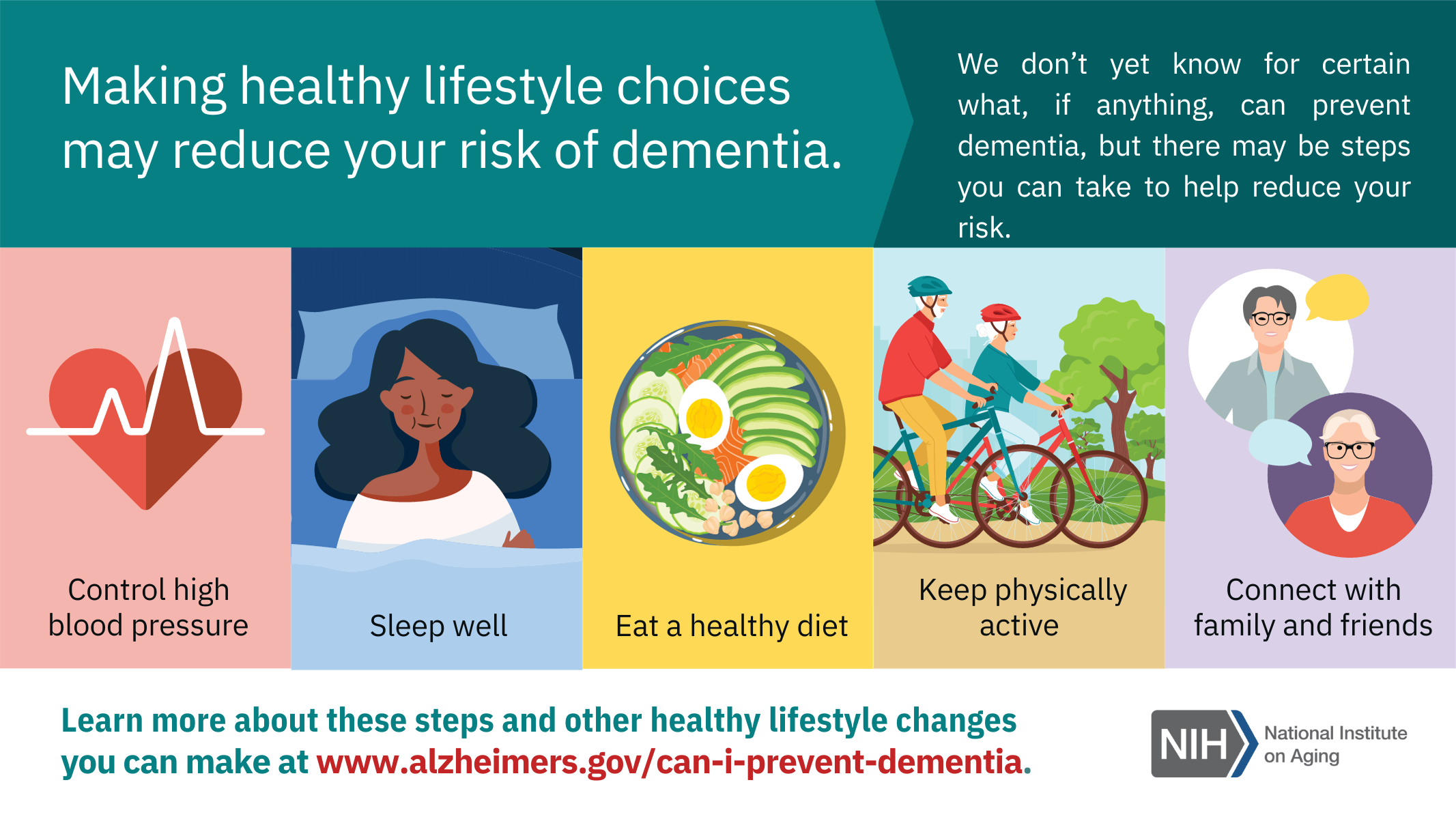
November was officially marked as Alzheimer’s Disease Awareness Month. Below are a few infographic resources available through the National Institute on Aging.

Mental health is a way of thinking that affects your thoughts and actions. It helps determine how you handle stress and relate to others. It is important at every life stage, from childhood and adolescence through adulthood. Mental health is just as important as your physical health because poor mental health that is not looked after can lead to some chronic health conditions over time.
Your mental health can change over time and can depend on the resources available to you. An example of this could be an individual who is experiencing economic hardship. As a result of their situation, they can experience poor mental health.
Some of the causes could be related to biological or genetic factors such as chemical imbalances in the brain. Some other causes could be early childhood traumas such as abuse, sexual assault or witnessing violence. Other factors that can lead to mental illnesses can be the excessive use of alcohol or drugs or feelings of prolonged isolation.
A “stigma” is a set of negative and unfair beliefs that a society or group of people have about something. Stigma can arise from a lack of understanding or inaccurate information about mental illness. As a society, we have made strides towards trying to reduce the negative view of those with mental illness, however there is always more work that can be done.
The best way for you to prevent stigma is by speaking openly about mental health. Educating yourself on the mental illness and getting informed can help reduce stigma. Showing compassion to your family or friends who are suffering also helps. For many mental health disorders, therapy and psychiatry have proven to be effective in reducing stigma and achieving well-being.
Elana Silverberg, MSW, Clinical Social Work Intern
September is Suicide Prevention Awareness Month. If you or someone you know needs help dial 988 for Mental Health Crisis and Suicide Prevention. Also, the National Suicide Prevention Lifeline is 1-800-273-TALK (8255) If the danger for self-harm seems immediate, call 911 right away. 
PREVENTION TIPS
 According to the National Institutes of Health (NIH), 35% of Americans who experience serious mental illness do not receive treatment; when we focus on those who experience substance use disorders the number is closer to 90% (Volkow et al., 2021). Given these high numbers it is crucial that we look for ways to remove barriers to accessing mental health care. While we often hear messages that promote the importance of mental health, there is also a long history in our society of treating mental illness and substance use as evidence of personal or moral failure. If we genuinely care about reducing the burden of mental illness on individuals, families, and society, then we must acknowledge that the stigma created by this mindset of mental illness and substance use as a character flaw can lead to barriers in accessing treatment for many people.
According to the National Institutes of Health (NIH), 35% of Americans who experience serious mental illness do not receive treatment; when we focus on those who experience substance use disorders the number is closer to 90% (Volkow et al., 2021). Given these high numbers it is crucial that we look for ways to remove barriers to accessing mental health care. While we often hear messages that promote the importance of mental health, there is also a long history in our society of treating mental illness and substance use as evidence of personal or moral failure. If we genuinely care about reducing the burden of mental illness on individuals, families, and society, then we must acknowledge that the stigma created by this mindset of mental illness and substance use as a character flaw can lead to barriers in accessing treatment for many people.
The language we use in our everyday lives can play a role in either adding to or reducing stigma around mental illness and substance use. For example, casual usage of words like “crazy’, “insane’, or “psycho” as pejorative descriptors in common conversation minimizes the significant challenges of those who experience mental illness and underscores the narrative that those with mental illness are somehow less worthy of being treated with respect and dignity.
Words used to describe people can influence not only how they view themselves but also the treatments they are offered. Studies have repeatedly shown that when patients are described as substance “abusers” or “addicts” physicians and other mental health clinicians are more likely to recommend punitive measures, such as jail time, instead of mental health treatment (Volkow et al., 2021). Using a term such as “substance use disorder” is clinically accurate and avoids the use of stigmatizing terms like “abuse” and “addiction”.
Many disability advocacy groups indicate a preference for the use of Person First Language (PFL) over the use Identify First Language (IFL) when describing diagnoses or disabilities that people experience. Using Person First Language to describe someone as a “person with Alcohol Use Disorder” instead of using Identity First Language to describe them as an “Alcoholic”, removes judgment and recognizes that the person is more than their diagnosis. However, not all populations have embraced Person First Language, and we should strive to use the terms preferred by those who experience a particular disability. One notable exception to the preference for Person First Language over Identity First Language relates to autism self-advocacy. In alignment with the Neurodiversity Movement, Identity First Language such as “autistic person” is overwhelmingly preferred by many autistic adults who consider the usage of Person First Language such as “person with autism” to be stigmatizing and invalidating of their lived experiences (Robison, 2019). They view autism as is intrinsic to their identity, not something that needs to be cured.
While it is always important to focus on the person not their diagnosis, it is also important to honor preferences about how certain individuals and populations prefer to describe themselves. The words we choose can either perpetuate stigma or honor the experiences of those who are struggling and need support.
Sarah Valerio, Clinical MSW Intern
References:
Robison, J.E. (2019), Talking about autism—thoughts for researchers. Autism Research, 12: 1004-1006.
Volkow, N. D., Gordon, J. A., & Koob, G. F. (2021). Choosing appropriate language to reduce the stigma around mental illness and substance use disorders. Neuropsychopharmacology.
The Administration for Community Living (ACL) is pleased to announce that the theme of Older Americans Month (OAM) 2021 is Communities of Strength. Older adults have built resilience and strength over their lives through successes, failures, joys, and difficulties. Their stories and contributions help to support and inspire others.
In May, ACL will celebrate the strength of older adults and the Aging Network, with special emphasis on the power of connection and engagement in building strong communities.
There are many things we all can do to nurture ourselves, reinforce our strength, and continue to thrive. Connecting with others is one of the most important—it plays a vital role in our health and well-being, and in that of our communities.
From finding joy in small things and sharing our stories, to looking at the big picture and giving to others, ACL will promote the ways we are connected and strong. Join us in encouraging people of all ages to celebrate their communities and community members.
 As an intern at JFCS, I have had the privilege of interacting with our senior clients during the coronavirus pandemic. Throughout a period of isolation, uncertainty, and fear, I have seen firsthand the resilience and positivity of older Americans. Whether I was assisting Senior Outreach Service (SOS) participants with the COVID vaccine pre-registration process, forming bonds with the Holocaust survivors through weekly check-in calls and Café Europa Zoom events, or delivering groceries to Healthy@Home clients, I have appreciated the opportunity to connect with older adults and learn about their life stories. My time at JFCS has taught me that older adults shape the communities they belong to by contributing wisdom, gratitude, and strength to those around them. As a young adult, I have benefited greatly from my relationships with JFCS’ older clients and will apply the lessons I have learned to my future career and personal life. This Older Americans Month, let us celebrate the invaluable role that older adults play in our communities.
As an intern at JFCS, I have had the privilege of interacting with our senior clients during the coronavirus pandemic. Throughout a period of isolation, uncertainty, and fear, I have seen firsthand the resilience and positivity of older Americans. Whether I was assisting Senior Outreach Service (SOS) participants with the COVID vaccine pre-registration process, forming bonds with the Holocaust survivors through weekly check-in calls and Café Europa Zoom events, or delivering groceries to Healthy@Home clients, I have appreciated the opportunity to connect with older adults and learn about their life stories. My time at JFCS has taught me that older adults shape the communities they belong to by contributing wisdom, gratitude, and strength to those around them. As a young adult, I have benefited greatly from my relationships with JFCS’ older clients and will apply the lessons I have learned to my future career and personal life. This Older Americans Month, let us celebrate the invaluable role that older adults play in our communities.
Emmanuelle Farrell, MSW Intern
We are so pleased to welcome Emmanuelle Farrell, Rutgers MSW student, to the agency for her first internship. She works with clients in Senior Services, Case Management and the Food Pantry and offers to help staff in any way she can. Despite these challenging times, she has already hit the ground running in the few months that she has been here.
Beverly Mishkin, LCSW, Director of Case Management & Senior Services
 Meet Emmanuelle!
Meet Emmanuelle!
My name is Emmanuelle Farrell, and I am interning at JFCS this year as part of my Master of Social Work program at Rutgers University. As a first-year graduate student, working at JFCS has offered me crucial experience with older adults and food insecure residents of Mercer County. As the COVID-19 pandemic has prevented many of my classmates from interning in person, I feel very grateful to be able to complete my internship in the JFCS office, where the few staff members working in-person wear masks and remain socially distant at all times. This direct approach has allowed me to see firsthand the significant impacts of the pandemic on the communities that JFCS serves.
The needs I have observed among the populations that JFCS provides services to appear to be exacerbated by financial, social, and health-related repercussions of the current pandemic. As I work primarily within the Senior Services department, I have noticed that older adults are in need of more than just basic necessities, like food and home health care. In making weekly check-in calls to Holocaust survivors and collecting seniors’ responses to program surveys, I have realized that many older adults are in dire need of companionship. This desire for social interaction has increased dramatically as the danger of contracting COVID-19 has stopped seniors from seeing family members and caregivers as frequently, if at all.
I also work with community members who reach out for assistance and help them get connected with our food pantry as a means of support.
I have also heard from other staff members that the demand for hunger prevention services has heightened significantly due to the widespread unemployment and subsequent economic difficulty associated with the pandemic. In general, the coronavirus pandemic has intensified the financial and interpersonal needs of vulnerable groups, increasing participation in JFCS’ programs and creating a unique learning environment for me as an intern.
There have been many connections between the content of my Master of Social Work courses and my experiences at JFCS. Primarily, I have been able to apply the communication skills I have learned in class to my interactions with clients, including empathetic listening and the use of furthering responses to encourage individuals to share. In addition, my work with the Holocaust survivors at JFCS has allowed me to implement a trauma-informed perspective, which I have learned about in my practice-focused classes. I greatly appreciate the opportunity to unite my academic setting with my fieldwork placement at JFCS.
Following the completion of my Master of Social Work degree, I hope to become a clinical social worker and administer therapy. Although I am interested in working with various populations, I intend to focus on serving trauma survivors through play therapy with children or cognitive behavioral therapy with adults. After becoming involved with JFCS, I have also gained an interest in working with older adults, particularly those who have endured trauma, such as survivors of the Holocaust. I plan to utilize many capabilities that I have developed as a JFCS intern in my future career, including performing intake procedures, researching program outcomes, and engaging compassionately with clients.
Although I have gathered many crucial sights throughout my time at JFCS, the most inspirational aspect of my internship has been the tangible difference that the organization makes in people’s daily lives. Every time I make a check-in call to an older adult, refer a new client to our food pantry, or assist with a distribution through the Mobile Food Pantry, I know I am making a meaningful change for an individual or family in need. I look forward to continuing my internship and furthering the agency’s incredible mission to empower individuals to care for themselves and others.
Emmanuelle Farrell, MSW Intern
 During the COVID-19 pandemic, many organizations, communities, and families have turned to Zoom as a way to connect virtually while remaining socially distant. But joining Zoom calls can be complicated and time-consuming, which discourages us from socializing with relatives and friends. These instructions can help you to join Zoom calls using a computer, a smartphone, or a regular cell phone so that you don’t miss out on virtual social gatherings.
During the COVID-19 pandemic, many organizations, communities, and families have turned to Zoom as a way to connect virtually while remaining socially distant. But joining Zoom calls can be complicated and time-consuming, which discourages us from socializing with relatives and friends. These instructions can help you to join Zoom calls using a computer, a smartphone, or a regular cell phone so that you don’t miss out on virtual social gatherings.
To minimize background noise, mute yourself when you are not speaking by clicking “Mute” on the bottom left hand corner of your Zoom screen
Stay Safe and Happy Zooming!
Emmanuelle Farrell, MSW Intern
 September is Hunger Action Month, a time to become educated on food insecurity and gain awareness on how you can help reduce its impact on our community. Although it may not be easily noticeable, food insecurity affects many communities, including Mercer County.
September is Hunger Action Month, a time to become educated on food insecurity and gain awareness on how you can help reduce its impact on our community. Although it may not be easily noticeable, food insecurity affects many communities, including Mercer County.
The United States Department of Agriculture (USDA) defines food insecurity as lacking consistent access to the amount of food needed to live a full and healthy life and is the product of both financial difficulty and inaccessibility to proper resources. Food insecurity is not always synonymous with poverty. As of 2017, the food insecurity rate in Mercer County was 10.6%, with 67% of the food insecure individuals being below the poverty threshold for government assistance and 33% not meeting the requirements for welfare benefits (Feeding America, 2018).
The COVID-19 pandemic has caused economic hardship for countless Americans, including those in our community. In Mercer County, the unemployment rate has increased from 3% in June 2019 to 12% in June 2020. In addition, the food insecurity in Mercer County is expected to rise to 13.6%, or over 50,000 people, by the end of 2020.
JFCS has seen the need rising first-hand with monthly visits to the on-site pantry doubling pre-pandemic numbers. Our Kosher Café, a nutrition site for low-income seniors to now receive grab-and-go meals, has seen a steady rate of attendance which is 25% higher than previous months.
How can you take action for Hunger Action Month?
If you are hungry, you are welcome.
If you are experiencing financial trouble and are seeking a food pantry near you, the JFCS pantry is open to all in the community who need help. We provide all clients with a supply of non-perishable items as well as fresh produce, cheese and chicken. All our clients also receive copies of the JFCS Pantry Newsletter which shares healthy, budget-friendly recipes centered on pantry staples along with other important information and resources.
We are currently providing pre-packed bags of groceries through no-contact pick up at our food pantry located on Alexander Road, Princeton NJ. You can arrange a pick-up time by calling us at 609-987-8100 Ext 237 or using our online sign up form.
Emmanuelle Farrell, MSW Intern
Hake, M., E. Engelhard, A. Dewey, C. Gundersen (2020). The Impact of the Coronavirus on Food Insecurity [Brief series]. Available from Feeding America.
US Department of Agriculture, (2019). Definitions of Food Security. Available online.
Feeding America. (2018). Food insecurity in Mercer County. Feeding America.
JFCS has always prided itself on providing a variety of internship experiences to high school, college and graduate school students. The ability to offer educational opportunities is an important part of our mission. We were particularly committed to continuing this practice during COVID-19. Through a combination of creativity and flexibility, students are participating, on a modified basis, in the agency’s existing programs and services. As a result, they have gained an additional perspective on how agencies must adapt their programs and respond to client needs during this pandemic. We are so appreciative to have such motivated and dedicated students interning at JFCS this summer.
Beverly Mishkin, LCSW, Director of Case Management & Senior Services
Meet Samantha!

My name is Samantha Goldfarb, and I am serving as an intern at JFCS this summer as a part of The College of New Jersey’s Summer Community Leaders program.
The summer is only halfway through and I have already recognized personal growth achieved through my new experiences. The COVID-19 pandemic has limited my scope of work, specifically face-to-face interactions with clients; yet, I have still been able to catch glimpses of the great community JFCS serves, from the friendliness of the Kosher Café attendees to the kind and good humored JFCS staff. Moments that have had the greatest impact include the look on our clients’ faces when they receive a bag of food and the excitement of community partners with whom we work to expand our outreach. If our community is this lively and connected now, I can only imagine how wonderful it is without social and spatial restrictions!
Where the altered programming has changed what I originally expected from an internship experience, I have also found it has afforded me unique opportunities I would not have had in a traditional internship placement. For example, I now have the opportunity to provide hands-on service work during a crisis while observing how a model organization can address the growing needs of its clients amid challenge and disorder.
My educational background is on disability rights and advocacy whereas the internship focuses on food security, nevertheless, my goal is to run a non-profit like JFCS one day, and any organization will have to be prepared to withstand any and all disasters that come its way. In this respect this modified internship is teaching me a lot about professional adaptability and how to best address problems as they arise. No organization could have been fully prepared for the demands of the pandemic, but this internship has shown me how a combination of flexible practices and a commitment to problem-solving allows an agency to stay on its feet and keep serving effectively.
I have seen the importance of helping employees connect with one another even if they have to be physically separated. I have seen an agency maintain its scope of service and level of impact by adapting programs to work within new limitations and focusing on building connections with other agencies to pool community resources.
While I regret missing out on some aspects of traditional service, I am very grateful for JFCS for teaching and modeling good practices for my work for years to come – and for still finding ways to sneak in moments with the community that make service so rewarding in the first place.
Samantha Goldfarb, Intern
With summer in full swing and the pandemic limiting the number of cool places people can retreat to, it is extra important to review the essentials of summer heat safety. These tips are good for everyone to keep in mind, but are tailored specifically for seniors whose additional needs are not always included in traditional heat safety reminders.

Samantha Goldfarb, Intern