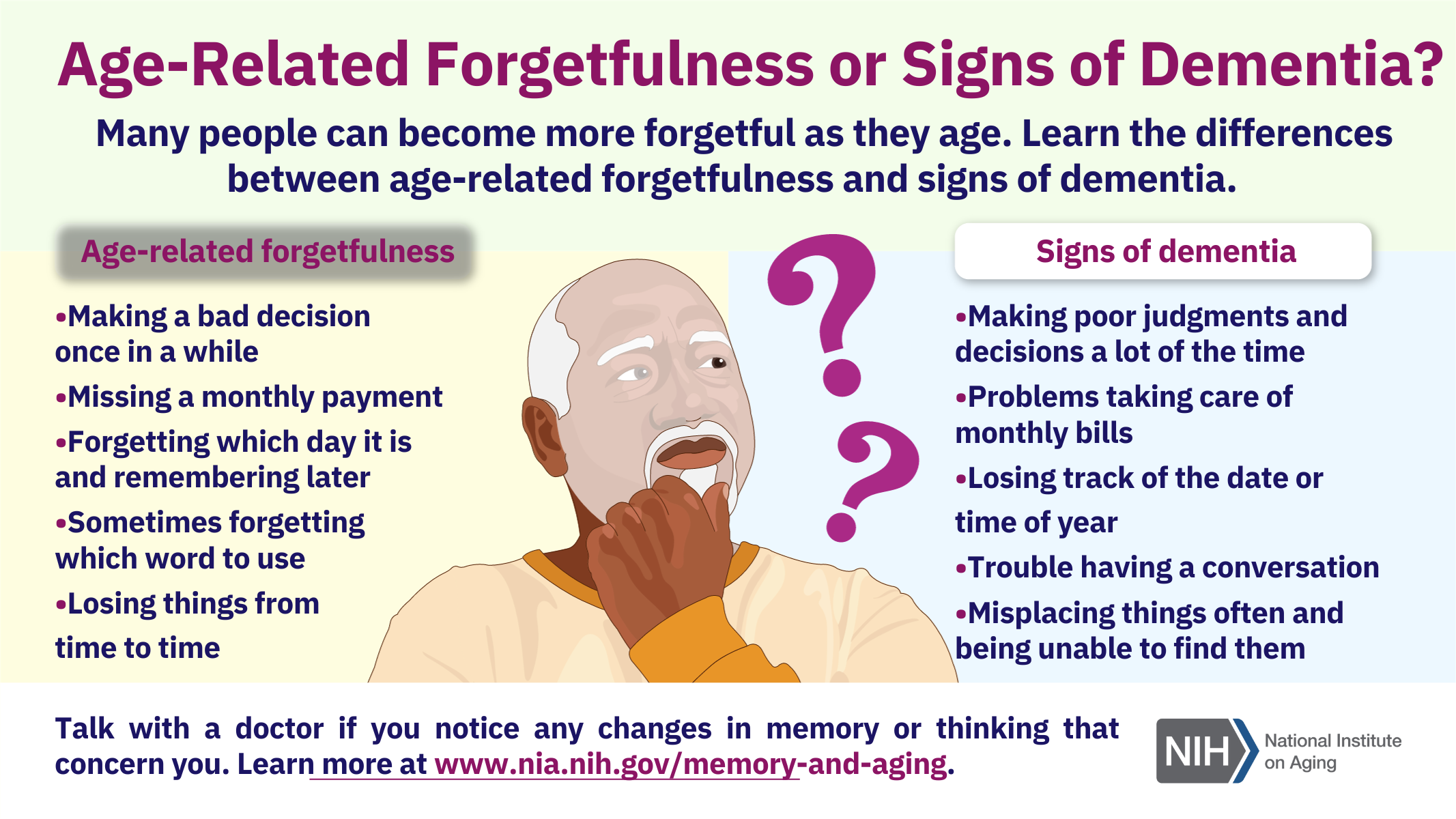
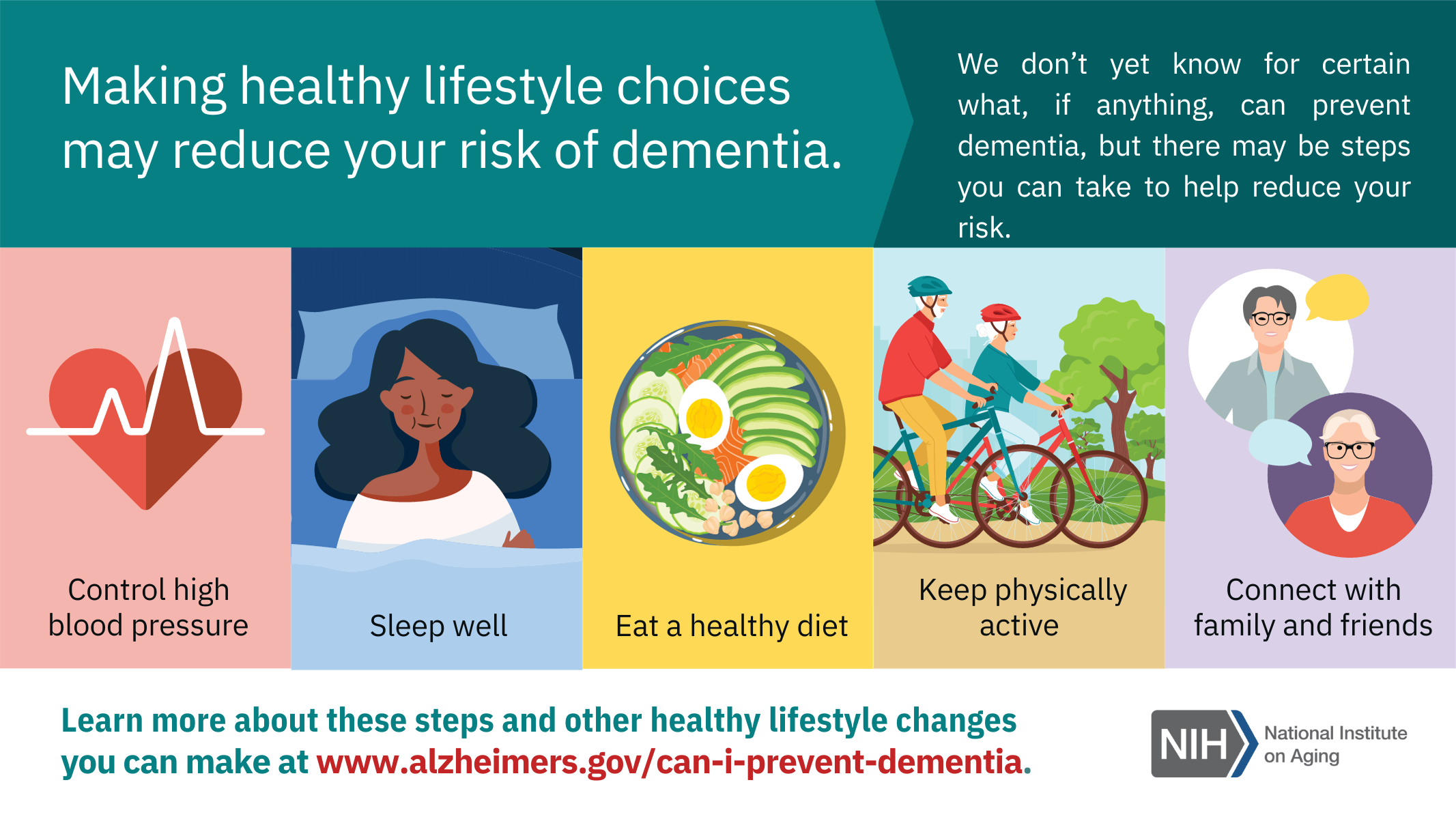
Resources for Alzheimer’s Disease Awareness
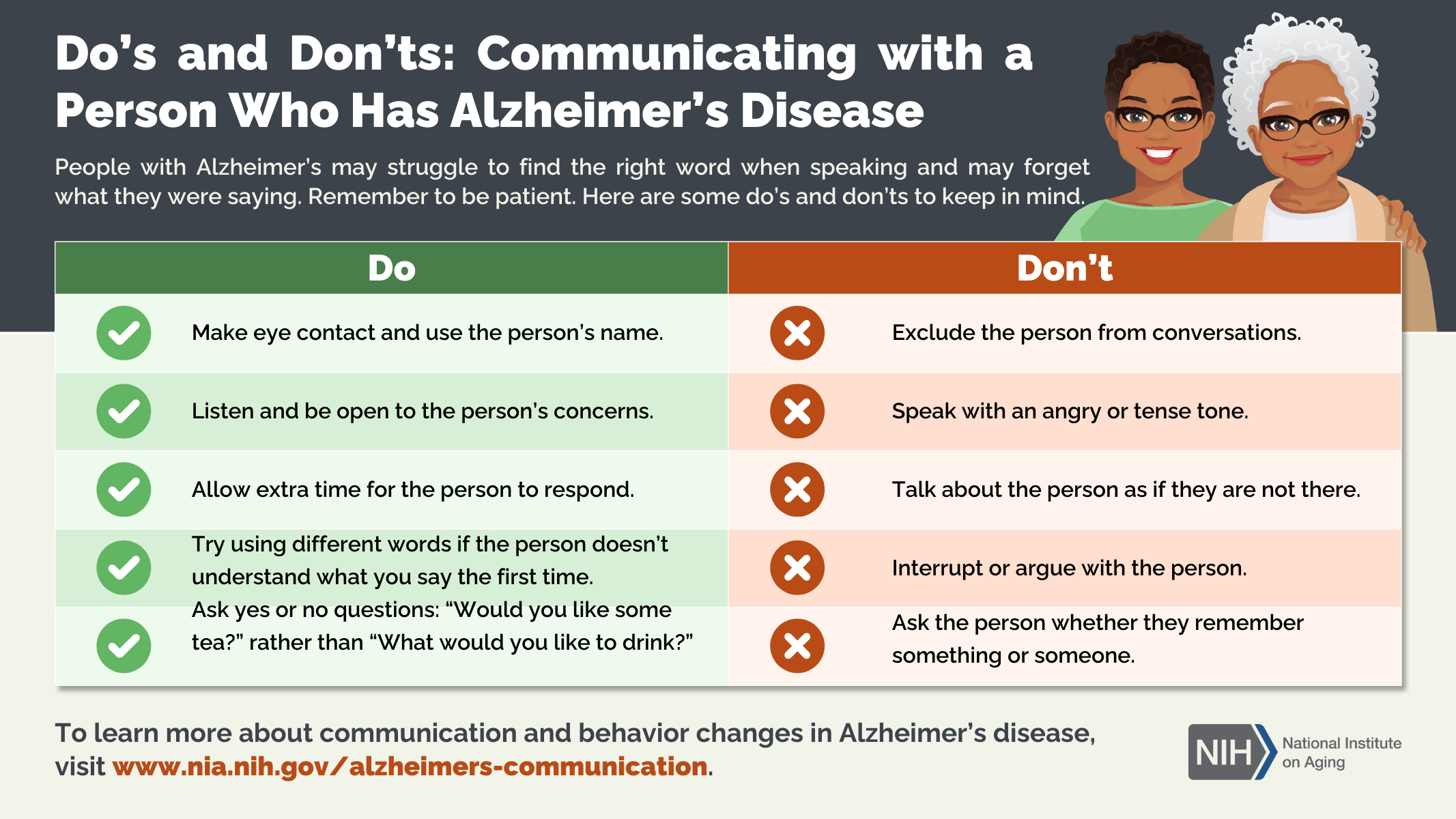
November was officially marked as Alzheimer’s Disease Awareness Month. Below are a few infographic resources available through the National Institute on Aging.
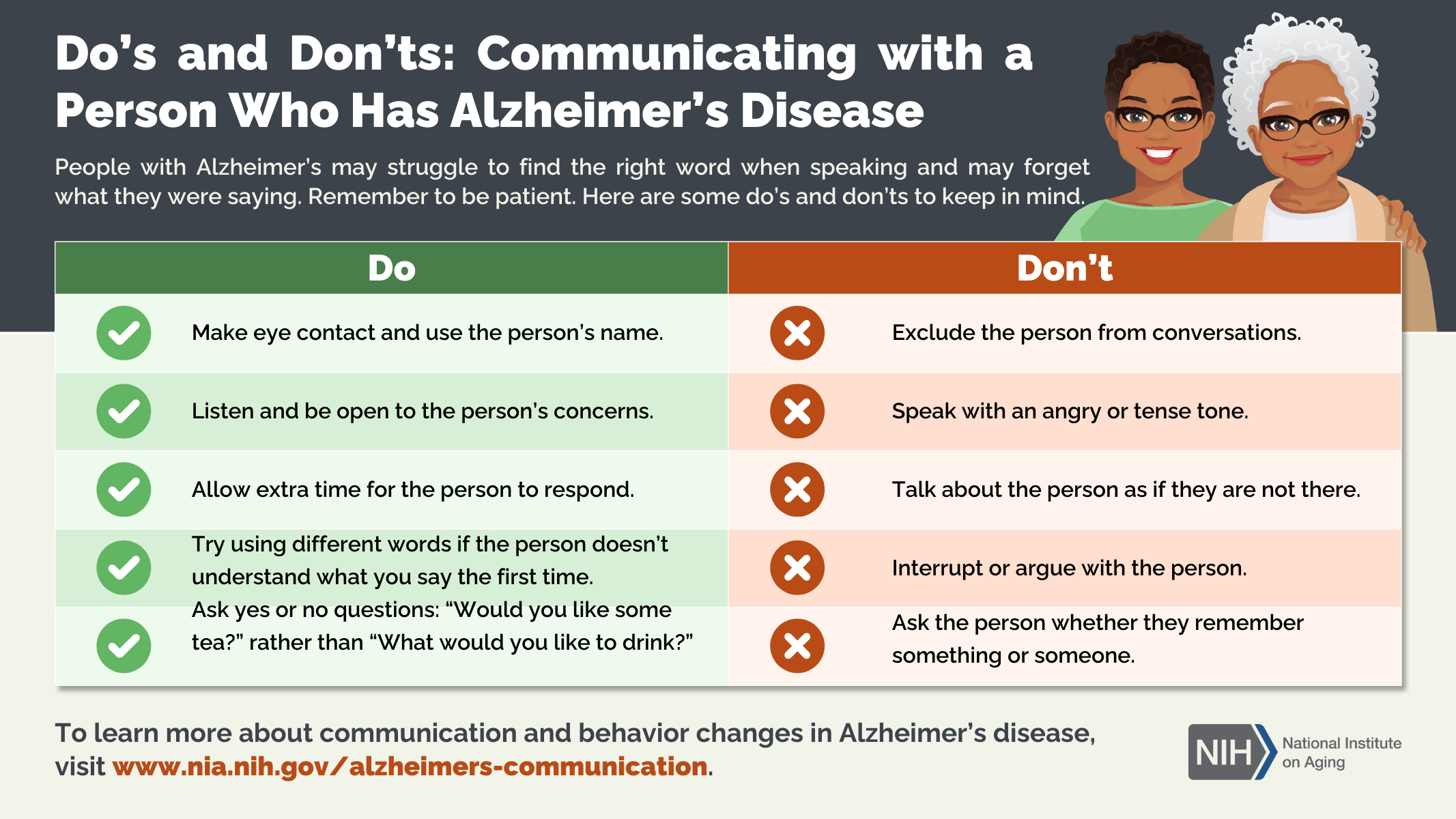
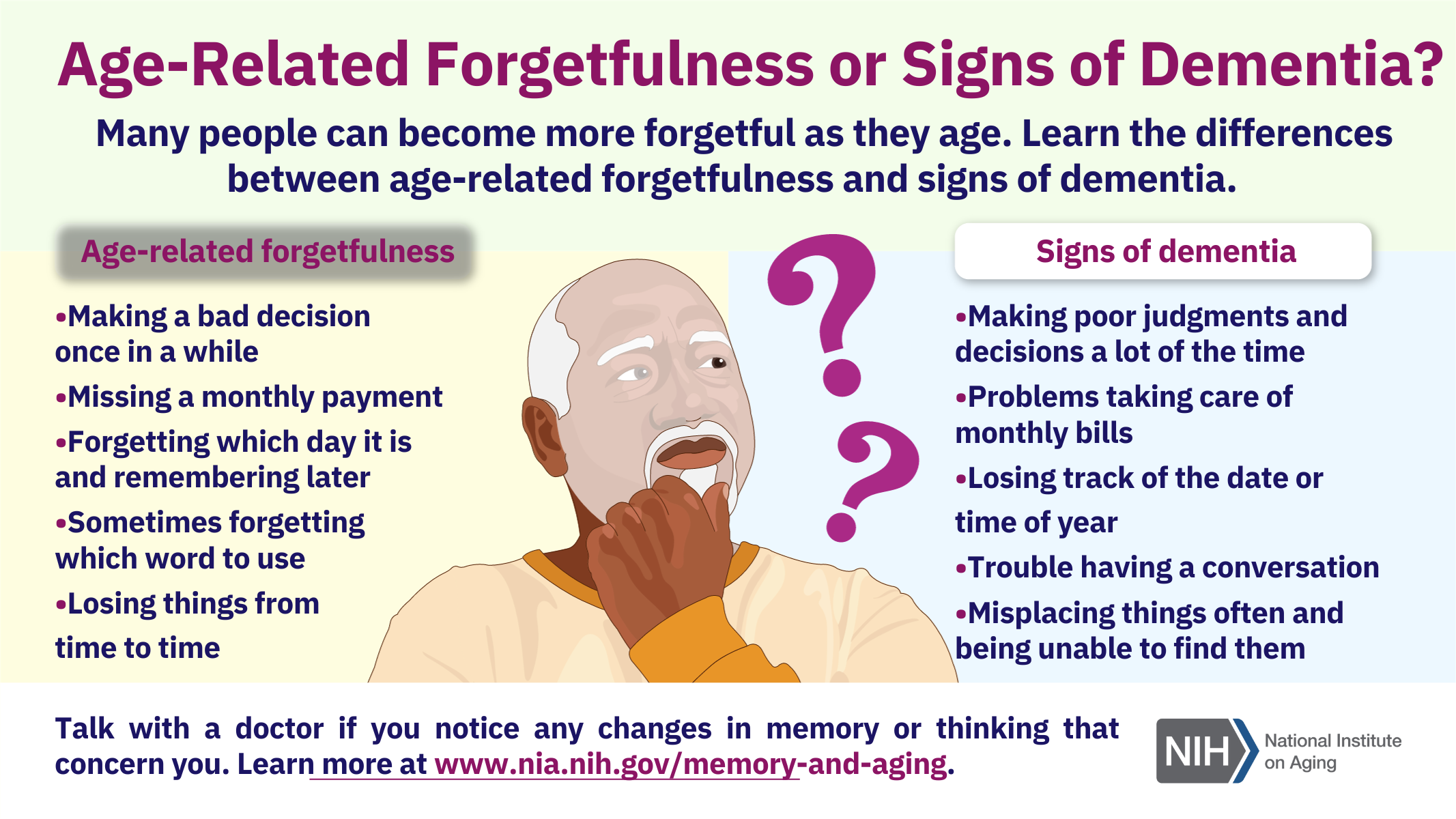

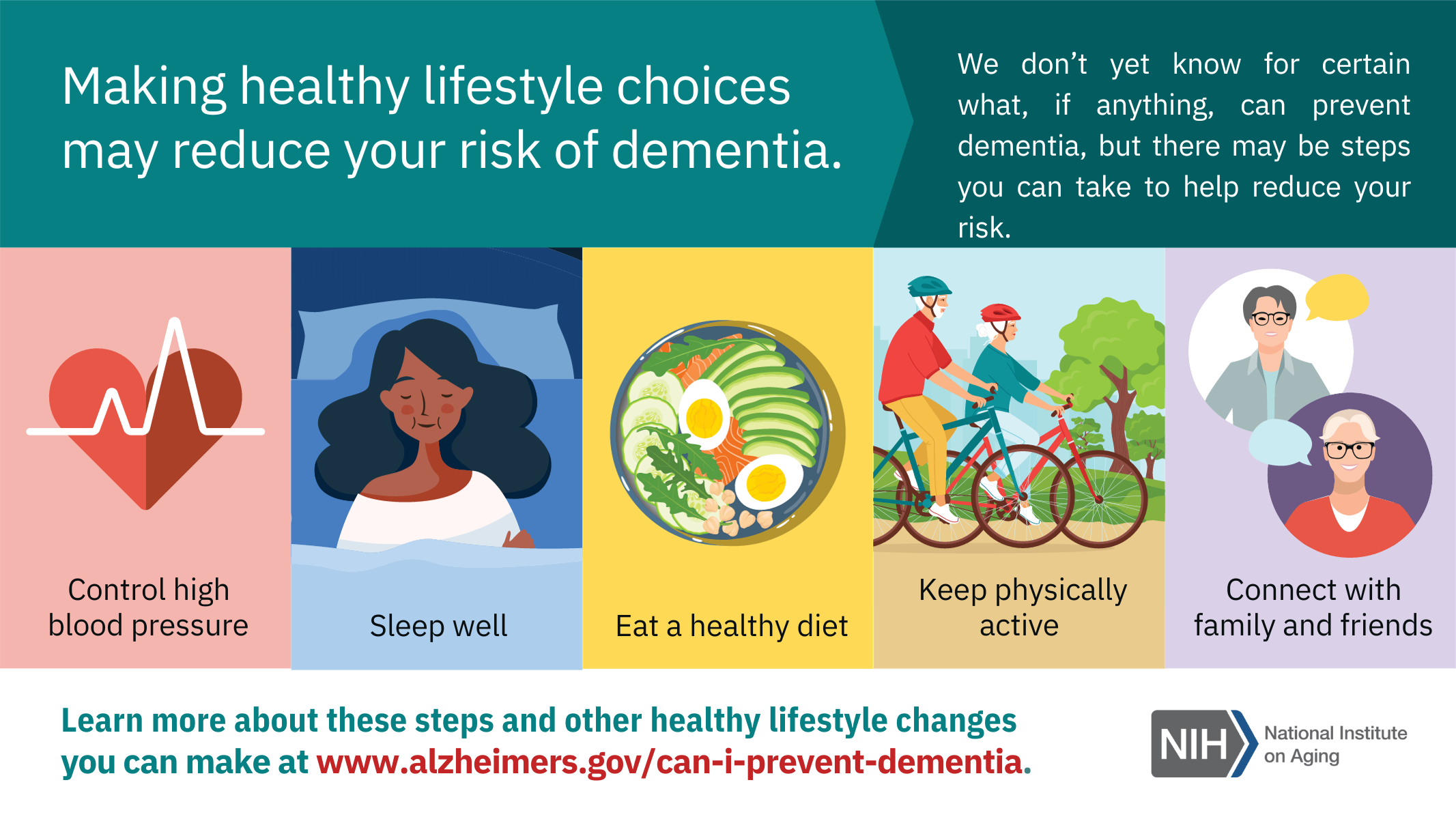
November was officially marked as Alzheimer’s Disease Awareness Month. Below are a few infographic resources available through the National Institute on Aging.

May is recognized as Older Americans Month and this year’s theme is “Age My Way” with a focus how seniors can plan to live safely and comfortably in their homes and communities for as long as possible. This is a core belief within the JFCS Senior Service program making us especially excited to share how we help our seniors age their own way.
The Administration for Community Living leads the national observance of Older Americans Month (OAM). OAM was established by President Gerald Ford in 1976 to recognize the contributions of older adults across the country and raise awareness of the needs specific to the aging demographic.
The 2022 theme for OAM is “Aging My Way” which provides an opportunity to highlight the many way older adults can safely remain in their communities in their golden years and the value they bring in being involved.
Aging-in-place support is one of the core focus areas of our senior service department. JFCS believes all individuals are entitled to their right to live their golden years as they choose. Our care managers help navigate the maze of senior care and assist seniors in making the best decisions for care, safety and comfort such as how to safely age in their homes, how to make informed decisions about assisted living, in-home care and plan for long-term medical, financial, and legal situations. Our team of geriatric care managers are here to serve as advocates for our clients, ensuring their needs are heard by family, caregivers, friends, doctors and professionals.
Beyond care management, JFCS even offers specific senior nutrition programs to ensure that older adults have access to nutritious food on a regular basis, further enhancing their quality of life in their later years.






The JFCS Friendly Caller & Visitor Program matches volunteers and seniors who feel more isolated or vulnerable, whether due to being homebound, living alone, or other circumstances. When COVID-19 forced many more seniors into isolation for their health & safety, JFCS continued this program matching more volunteers with more seniors.
Two volunteers shared their perspective on what these regular connections have meant to them, and the senior they connect with.
I’ve fostered a deep, meaningful, and humorous relationship through my friendly, weekly calls with Ms. Jane. Our calls are centered around positivity, compassion, and encouragement, whether it be a new hobby or to explore a new museum. This has greatly abated the fear of isolation and promoted social connection.
Ms. Jane looks forward to our weekly calls, to the point where the excitement and enthusiasm is palpable; an experience that is beyond rewarding.
I continue to speak with Ruth weekly. Our conversations have no topic; we speak as two friends about family, books, happenings in our lives, and reminiscences. She picks the topics, sets the tone and pace. I follow her direction.
I know Ruth feels lonely, and our talks provide relief each week. I can tell that she looks forward to and enjoys our conversations, for she says so repeatedly and thanks me each week.
*all names changed for confidentiality
 When matching an aide to a client, it does help to know as much as possible. Understand that the caregiver and you may take several days to settle into a routine and that the first day may not be a good reflection on how good the match is. Agencies will do the best they can to match an aide based on skill set and caregiver availability to meet your needs. A creative solution, such as slightly different hours, may be offered by the agency if the caregiver they think would be best has availability that slightly differs from your initial request.
When matching an aide to a client, it does help to know as much as possible. Understand that the caregiver and you may take several days to settle into a routine and that the first day may not be a good reflection on how good the match is. Agencies will do the best they can to match an aide based on skill set and caregiver availability to meet your needs. A creative solution, such as slightly different hours, may be offered by the agency if the caregiver they think would be best has availability that slightly differs from your initial request.
Since the pandemic, many agencies now require a minimum of 16-20 hours per week of care due to the high demand for caregivers; many have had to increase their hourly rate from approximately $26 to $30, and many have increased the hourly block from 3 or 4 hours to 6-hour shifts. The minimum number of days care is given may have also been adjusted due to availability of staff. If you have a request for a shorter block of time or less frequency, you may have a greater turnover in aides being assigned to your care. In general, the more hours and days per week, the more consistent the caregiver. Each agency sets its own policy regarding rates and minimum care.
Not all agencies require their caregivers/staff to be vaccinated. We advise you to inquire about the status of your caregiver. Please know that the agencies do provide masks, gloves and sanitizers for their aides to use.
Generally, most agencies do not bring caregivers to your home to be “interviewed” prior to the assignment. The agency will match the best caregiver to your needs and if the match does not meet your expectations after several days, the agency will do its best to make any necessary changes. Most aides do not have interviewing experience and may not present his or her best version of oneself in that type of setting. If you are being discharged from a rehab setting, the agency can, in most cases, bring the aide to the facility for “training” by the PT department regarding any specific needs.
Following a hospitalization or rehabilitation stay, the agency may recommend having “round the clock” care for the first few days. This means you will be billed the hourly rate x 24, per day. The benefit of this is that your overnight needs can be evaluated so that you are safe, especially if there is concern about being a fall risk or having impaired sleep and needing care throughout the night. The agency will generally arrange for (2) 12-hour shifts, or (3) 8 hour shifts of aides. Once it is determined that you or your loved one is not at risk of falling at night, or is able to sleep through the night, the schedule can be adjusted to your needs.
If you require a caregiver who has his/her own car or has a driver’s license (and can drive your car) to do errands, take you to a doctor appointment, etc., please tell the agency. Not all aides have a car and/or a driver’s license.
If you need a live-in caregiver, keep in mind the caregiver needs to sleep and cannot work “round the clock”. Live-in aides are required to have 5 hours of consecutive hours of sleep, with 8 hours total per night, as mandated by labor laws. If the client needs brief help more than once or twice nightly, additional overnight support may be necessary; either a second aide can be added to remain awake overnight or two twelve hour shifts of care may need to be implemented in lieu of live-in care.
If you have a live-in caregiver, you will need to provide a separate room for him/her for sleeping in addition to providing food. Any unusual or special dietary requests by the caregiver are not your responsibility to provide.
Most agencies will charge time-and-a-half on holidays.
If you have a pet in the house, you need to inform the home care agency and do not assume that the caregiver will take care of your pet (walk, feed, clean litter box, etc.).
We hope you find this information useful. If you would like to speak to a geriatric care manager, please contact JFCS at 609-987-8100.
Beth Hammer, LCSW Geriatric Care Manager
Andrea Gaynor, LCSW Geriatric Care Manager
Beverly Mishkin, LCSW Director of Senior Services
The federal tax filing season began this week and threat actors are quickly targeting taxpayers. The NJCCIC observed phishing campaigns attempting to be delivered to New Jersey State employees, with the intent to download and install malware. Threat actors spoofed the sender’s display name to a known source or entity to convince the recipient to trust the email without verifying its legitimacy. The sender’s display name is purported to be from the Internal Revenue Service (IRS); however, upon further inspection, the sender’s domain name was “irs.com” instead of the legitimate “irs.gov.” Additionally, the email signature claimed to be the “Government department” in the IRS to add a false sense of legitimacy and authority.
The subject line displayed “Information Regarding Your Tax Form” to convince their target to open the email and take action. Although the email referenced an attached “TAXFORM.pdf,” it contained an attached Microsoft Word name “Tax Form.doc” that, if clicked, downloads and installs malware. In addition to the IRS, threat actors may also spoof popular tax brands to trick their victims into divulging sensitive information, which can then be used to file fraudulent tax returns, collect refunds, and engage in other identity theft schemes. Additionally, companies required to provide customers with tax documents may also be impersonated in attempts to convince victims into opening malicious links or attachments.

The NJCCIC recommends users and organizations educate themselves and others on these continuing threats and tactics to reduce victimization. The IRS does not initiate contact with taxpayers by email, text messages, or social media channels to send or request personal or financial information. Please review the NJCCIC Product Beware of Tax Scams to learn more about common tax scams—including tax identity theft, IRS impersonation scams, and fraudulent tax preparer scams—and cybersecurity best practices to help protect your identity, data, and tax refunds. Additional tax scams and consumer alerts can be found on the IRS website.
The end of year is always a time to reflect and set goals for the year ahead. JFCS is sharing inspiring stories of how our programs have helped the individuals, families and community we serve move forward after another challenging year for all.
Valerie reached out to JFCS after recognizing the severity of the anxiety and depression she was experiencing. After making the commitment to counseling and putting new skills into action, Valerie felt empowered to address the root of her most severe symptoms – low self-esteem caused by lack of boundaries in challenging relationships. By tackling the causes of her anxiety and depression, Valerie soon felt confident to move forward from therapy.
“My counselor was exceptional and did an excellent job listening without judgment and providing professional support. I am extremely grateful for this experience and am looking forward to moving past my anxiety.”

The JFCS senior service team received a call from Arthur, who lives out of state, and was concerned about his 90 year-old mother who lives alone in the Princeton community. While the son was in town, one of our geriatric care managers scheduled an appointment to meet with both Arthur and his mother, Ruth. The care manager did a thorough assessment including home safety, social supports, meal shopping/preparation and transportation options. A plan of care was developed to address these issues. Arthur left for home feeling like a “weight had been lifted from his shoulders.”
He knew he was no longer alone to deal with the challenges that lie ahead. JFCS receives many calls like this and our expert team of geriatric care managers is available to provide guidance and support to those in similar situations.

Melinda is a grandmother who serves as the primary guardian to both grandsons. She lives on a fixed income and is the full-time caregiver to both children, one of whom has significant physical special needs, requiring in-home therapy and care. It is difficult for Melinda to get out of the house, but thankfully, she is in counseling with one of our JFCS therapists who referred her to the pantry team. Our pantry team was able to identify one of our local mobile food pantry stops where Melinda can easily and conveniently pick up groceries. Melinda was also able to receive gift cards through the LIGHTS program so she could purchase holiday gifts for her grandsons, something out of reach without this support.

“With a resource coming right to my neighborhood, it is a huge relief. I face serious financial challenges as the sole caregiver for my grandsons, and I am so appreciative of any help. Even the smallest gesture makes a big difference in our lives.”
Stories like those of Valerie, Arthur, Ruth and Melinda are just some examples of the impact we have made, together, over the past year. You can read further about how JFCS has served the community this year in our latest Annual Report.
We thank all of those who have supported us, especially in these ongoing, challenging times. We hope you can once again trust JFCS to care for those in need with an end of year gift. Help us move into the new year with help, hope & healing.
 At JFCS we are always available to provide care for the Caregivers:
At JFCS we are always available to provide care for the Caregivers:
Contact Beverly Mishkin, Director of Senior Services, beverlym@jfcsonline.org or Chaplain Beverly Rubman, beverlyr@jfcsonline.org, for more information.
We share several readings below to support you as you take care of your loved ones…
When despair grows in me
and I wake in the middle of the night at the least sound
in fear of what my life and my children’s lives may be,
I go and lie down where the wood drake
rests his beauty on the water, and the great heron feeds.
I come into the peace of wild things
who do not tax their lives with forethought
of grief. I come into the presence of still water.
and I feel above me the day-blind stars
waiting for their light. For a time
I rest in the grace of the world, and am free.
–Wendell Berry–


Dear God, give me the strength to face this day,
To deal with the tension, anxiety and dizzying confusion of my life.
Teach me to focus, to prioritize, to see with clarity.
God of patience, teach me to be patient.
Forgiving God, teach me to forgive.
Bless me with the courage to face my loved one’s illness and pain, amidst my own fears.
Touch me with your spiritual light, your love, your wisdom
So that I can continue my task tomorrow, knowing that You are by my side.
–Based on the writing of Rebbe Nachman of Breslov, appearing in The Gentle Weapon: Prayers for Everyday and Not-So-Everyday Moments (Jewish Lights)–
“It’s funny: I always imaged when I was a kid that adults had some kind of inner toolbox, fully of shiny tools: the saw of discernment, the hammer of wisdom, the sandpaper of patience. But then when I grew up I found that life handed you these rusty bent old tools—friendships, prayer, conscience, honesty—and said, Do the best you can with these, they will have to do. And most, against all odds, they’re enough.”
–Anne Lamott, Traveling Mercies: Some Thoughts on Faith, page 103–


Sometimes a bird will sing at midnight.
Perhaps restless, perhaps confused,
Perhaps so full of joy and love
That music bursts forth.
Fill me with song on sleepless nights.
Fill me with music in the lonely deep.
Let the promise of a new day
Bring comfort and consolation.
–Alden Solovy, This Grateful Heart—
When so many traditions and observances are focused around the gathering of family and friends, it can be especially hard to celebrate when grieving the loss of a loved one. Our Handling the Holidays series is held ahead of the major Jewish holidays, Passover, Yom Kippur & Rosh Hashanah, and Hanukkah, to help those who are grieving.
 Light in the Midst of Darkness: Chanukah for those who are bereaved
Light in the Midst of Darkness: Chanukah for those who are bereaved
Join for a one-time virtual support group to help you through the dark days of this difficult year. Facilitated by Chaplain Beverly Rubman.
No fee to attend, advance registration required.
Our senior service team shared their thoughts and experiences working with our older adults clients over the past year – everything from how seniors adapted to quarantine and supported each other, to how Holocaust Survivors maintained their connections while learning to Zoom.
The Administration for Community Living (ACL) is pleased to announce that the theme of Older Americans Month (OAM) 2021 is Communities of Strength. Older adults have built resilience and strength over their lives through successes, failures, joys, and difficulties. Their stories and contributions help to support and inspire others.
In May, ACL will celebrate the strength of older adults and the Aging Network, with special emphasis on the power of connection and engagement in building strong communities.
There are many things we all can do to nurture ourselves, reinforce our strength, and continue to thrive. Connecting with others is one of the most important—it plays a vital role in our health and well-being, and in that of our communities.
From finding joy in small things and sharing our stories, to looking at the big picture and giving to others, ACL will promote the ways we are connected and strong. Join us in encouraging people of all ages to celebrate their communities and community members.
 As an intern at JFCS, I have had the privilege of interacting with our senior clients during the coronavirus pandemic. Throughout a period of isolation, uncertainty, and fear, I have seen firsthand the resilience and positivity of older Americans. Whether I was assisting Senior Outreach Service (SOS) participants with the COVID vaccine pre-registration process, forming bonds with the Holocaust survivors through weekly check-in calls and Café Europa Zoom events, or delivering groceries to Healthy@Home clients, I have appreciated the opportunity to connect with older adults and learn about their life stories. My time at JFCS has taught me that older adults shape the communities they belong to by contributing wisdom, gratitude, and strength to those around them. As a young adult, I have benefited greatly from my relationships with JFCS’ older clients and will apply the lessons I have learned to my future career and personal life. This Older Americans Month, let us celebrate the invaluable role that older adults play in our communities.
As an intern at JFCS, I have had the privilege of interacting with our senior clients during the coronavirus pandemic. Throughout a period of isolation, uncertainty, and fear, I have seen firsthand the resilience and positivity of older Americans. Whether I was assisting Senior Outreach Service (SOS) participants with the COVID vaccine pre-registration process, forming bonds with the Holocaust survivors through weekly check-in calls and Café Europa Zoom events, or delivering groceries to Healthy@Home clients, I have appreciated the opportunity to connect with older adults and learn about their life stories. My time at JFCS has taught me that older adults shape the communities they belong to by contributing wisdom, gratitude, and strength to those around them. As a young adult, I have benefited greatly from my relationships with JFCS’ older clients and will apply the lessons I have learned to my future career and personal life. This Older Americans Month, let us celebrate the invaluable role that older adults play in our communities.
Emmanuelle Farrell, MSW Intern
JFCS continues to provide an updated list of known vaccine sites on our COVID resource page. We are making every effort to keep the community up to date through the resource page with information available to us.
Our senior services team is working to connect our clients, specifically our senior clients and others who currently qualify for vaccine, to any available and known resources.
Anxieties are reaching a peak level amongst the older adults in our community as the state-wide scramble for vaccine appointments drags on. For members of JFCS Secure@Home and Senior Outreach Service (SOS) programs, there is some solace found in the dedication and compassion of our geriatric care managers.
Our senior service team is going above and beyond for our Secure@Home members and senior clients. We know many older adults are facing challenges securing a vaccine timeslot. For Secure@Home members, the 24/7 support and hard work of our team of geriatric care managers has been the difference between getting a timeslot and not. Members of the program regular updates from the care managers about all available vaccine resources. The up-to-date information has helped many of our program members be connected with vaccine distribution sites and confirm appointments.
During the past year, when many seniors were more isolated and distanced from loved ones than ever before, our senior services team ensured they never felt alone. Whether it was a friendly check-in needed, or finding a volunteer to help with groceries, or helping find and secure COVID-19 tests or vaccine appointments, our care managers were there for our members. The team continues to respond to the immediate needs of seniors with each wave of challenges during the pandemic.
“I keep thinking how many thanks I’m feeling for getting that [registration] link to me. I almost lost an appointment within the next few weeks but was able to book one thanks to your quick action!”
“You both put the arms of angels around me this morning. Thank you for helping me find an appointment for today. Sunny day. Easy trip. Very, Very well-organized site. Date for next vaccine set.”
“I am emailing to commend Beth Hammer for her extraordinary efforts to get vaccination appointments for me and other Secure@Home members. She has done far more than what I would expect her to do. And it has worked. Thank you for having such a dedicated and determined staff member!”
 Our geriatric care managers are here to help you and your loved ones by providing an umbrella of services to promote healthy aging and “aging in place.” Full Secure@Home membership benefits include care management, assessment, 24/7 emergency phone availability, information & referral, transportation options, monthly hellos and more. Geriatric care consultations and care management can also be provided at an hourly rate if you are not yet in need of full-time support but as-needed care.
Our geriatric care managers are here to help you and your loved ones by providing an umbrella of services to promote healthy aging and “aging in place.” Full Secure@Home membership benefits include care management, assessment, 24/7 emergency phone availability, information & referral, transportation options, monthly hellos and more. Geriatric care consultations and care management can also be provided at an hourly rate if you are not yet in need of full-time support but as-needed care.
When it can be difficult to find peace of mind, our Secure@Home team is providing comfort and solace to seniors during this pandemic and beyond. If you want to learn more about Secure@Home and our senior support programs, contact our team at 609-987-8100 Ext 203.